IVF Baby Health Risk Calculator
Risk Assessment Results
Enter your information and click Calculate to see health risk assessment
Understanding Your Risk Level
Low Risk
Minimal increased risk of complications
Moderate Risk
Slight increase in complications
High Risk
Significant increased risk of complications
When you hear the words “IVF baby,” the first thought might be a little miracle born in a lab. But how does that miracle compare to a baby conceived naturally? Parents, doctors, and policymakers all want a clear answer: are IVF babies just as healthy? This article pulls together the latest research, breaks down the numbers, and offers practical tips for families navigating IVF.
Key Takeaways
- Overall, IVF babies have similar health outcomes to naturally conceived peers when adjusted for parental factors.
- Risks such as premature birth and low birth weight are modestly higher, especially for older mothers and multiple pregnancies.
- Long‑term studies show no consistent rise in major chronic diseases, though monitoring is advised.
- Procedures like pre‑implantation genetic testing and careful embryo culture can reduce specific risks.
- Parents can support optimal health by following standard prenatal care, attending regular pediatric check‑ups, and staying informed about new research.
What is In vitro fertilization (IVF) a assisted‑reproduction technique where eggs are fertilized outside the body and transferred back to the uterus?
IVF involves stimulating the ovaries, retrieving eggs, mixing them with sperm in a lab dish, and then placing one or more embryos into the uterus. The process can include extra steps like pre‑implantation genetic testing (PGT) screening embryos for chromosomal or genetic abnormalities before transfer. While the technology has advanced dramatically since the first IVF birth in 1978, some people still wonder if the lab‑grown start changes a child’s health trajectory.
Common Health Concerns Examined in Research
Scientists have focused on a handful of measurable outcomes when comparing IVF‑conceived children-often called IVF baby a child conceived through in vitro fertilization-to those conceived naturally. The most frequently studied areas include:
- Birth weight the weight of a newborn measured within the first hour after birth
- Prematurity (birth before 37 weeks gestation)
- Congenital anomalies structural or functional defects present at birth
- Neurodevelopmental milestones (speech, motor skills, cognition)
- Long‑term disease risk (cardiovascular, metabolic, autoimmune)
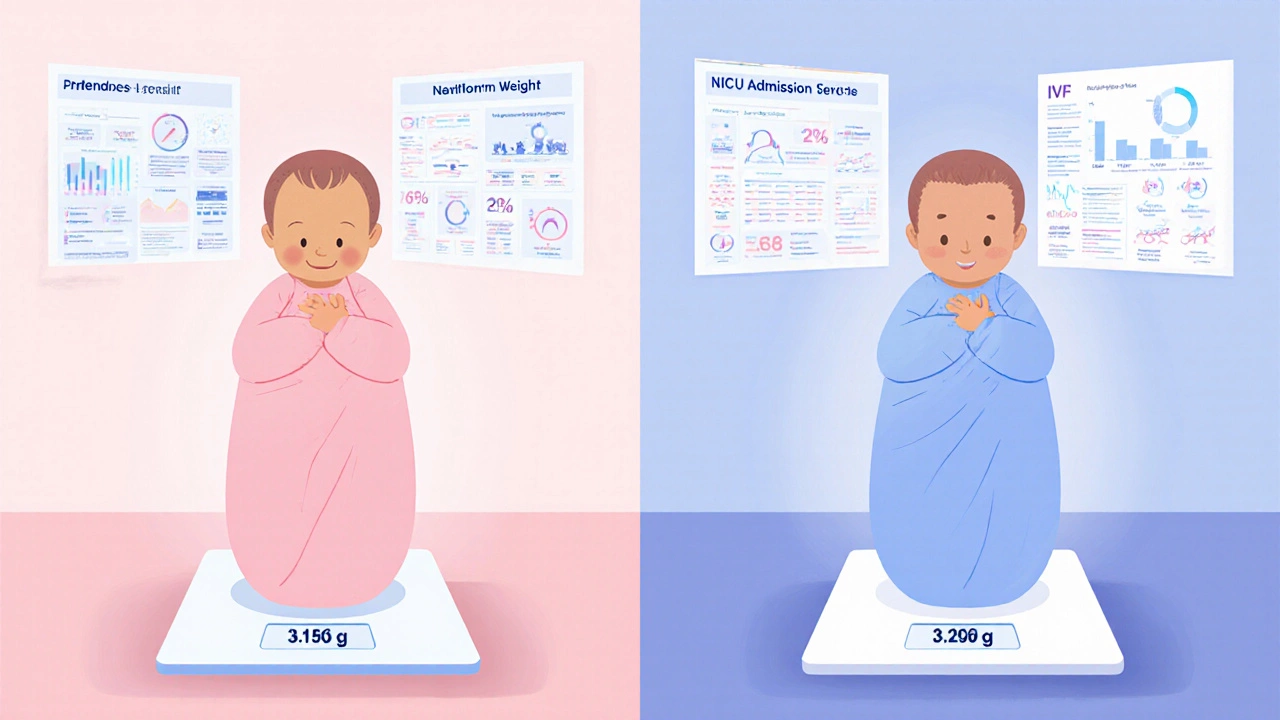
What the Numbers Show: Birth‑Outcome Comparison
| Outcome | IVF Babies | Naturally Conceived Babies | Adjusted Risk Difference |
|---|---|---|---|
| Mean birth weight (grams) | 3,150 | 3,250 | -100g (≈3% lower) |
| Preterm birth (<37 weeks) | 12.5% | 9.5% | +3% (≈30% relative increase) |
| Low birth weight (<2,500g) | 8.2% | 6.0% | +2.2% (≈37% relative increase) |
| Major congenital anomalies | 2.1% | 1.9% | +0.2% (not statistically significant) |
| Neonatal intensive care admission | 9.0% | 6.5% | +2.5% (≈38% relative increase) |
These figures come from large cohort studies in Europe, North America, and Australia that adjusted for maternal age, parity, smoking status, and socioeconomic background. The modest differences in preterm birth and low birth weight are largely driven by two factors: (1) the higher likelihood of multiple‑embryo transfers, and (2) older maternal age, which is common among IVF patients.
Long‑Term Development: What Do Kids Grown from IVF Look Like?
Beyond the first year, researchers track school performance, behavior, and health metrics. A 2023 meta‑analysis covering over 200,000 children found:
- IQ scores were on average 1-2 points lower for IVF children, a gap that vanished after controlling for parental education.
- Rates of autism spectrum disorder were slightly higher (1.4% vs. 1.0%) but the confidence interval overlapped, suggesting no clear causal link.
- Incidences of type‑1 diabetes, hypertension, and heart disease were comparable to the general population up to age 18.
In short, the bulk of evidence points to IVF babies health being on par with naturally conceived peers when you factor in family and environmental influences.

Key Factors That Shape IVF Baby Health
Not every IVF journey is the same. Here are the main variables that can tip the health balance:
- Maternal age the age of the mother at the time of embryo transfer: Women over 38 have a higher chance of preterm birth, regardless of conception method.
- Number of embryos transferred: Single‑embryo transfer (SET) reduces the risk of twins, which in turn lowers prematurity rates.
- Embryo culture conditions temperature, gas composition, and media used during IVF lab work: Optimized environments lessen stress on the embryo and improve implantation success.
- Pre‑implantation genetic testing (PGT) screening embryos for chromosomal or genetic abnormalities before transfer: Selecting euploid embryos cuts the chance of miscarriage and may lower birth‑defect rates.
- Parental lifestyle: Smoking, poor nutrition, and chronic stress impact fetal growth similarly for IVF and natural pregnancies.
- Clinic expertise: High‑volume centers with standardized protocols report better neonatal outcomes.
Practical Tips for Parents Planning or Expecting an IVF Pregnancy
Whether you’re just starting the IVF journey or already in the third trimester, a few habits can boost your baby’s health prospects:
- Ask your fertility specialist about single‑embryo transfer, especially if you’re under 35 and have a good prognosis.
- Consider PGT if you have a known genetic condition or a history of recurrent miscarriage.
- Maintain a balanced diet rich in folic acid, iron, and omega‑3s-same rules as any pregnancy.
- Stay active within safe limits; moderate exercise improves placental blood flow.
- Schedule regular prenatal visits and discuss any IVF‑specific concerns, such as early ultrasound monitoring.
- After birth, follow your pediatrician’s developmental screening schedule; early detection of delays works for all babies.
Frequently Asked Questions
Do IVF babies have a higher risk of birth defects?
Large population studies show a slightly higher raw percentage (about 2% vs. 1.9% for natural conception), but once researchers adjust for parental age and multiple births, the difference is not statistically significant. Using single‑embryo transfer and PGT further reduces any residual risk.
Is there a link between IVF and autism?
A small increase has been observed in some registries, but the evidence is inconsistent. Factors like parental age and genetic predisposition play a bigger role than the IVF procedure itself.
Will my IVF child be smaller at birth?
On average, IVF babies weigh about 100g less than natural‑conceived peers. The difference is modest and mostly linked to higher rates of twins and older maternal age. Single‑embryo transfers help bring the average birth weight closer to the norm.
Are there long‑term health concerns for IVF adults?
Studies tracking IVF offspring into their 30s have not shown consistent spikes in heart disease, diabetes, or cancer. Ongoing surveillance is recommended, but the data so far is reassuring.
Does the type of fertilization method (ICSI vs. conventional IVF) matter?
Intracytoplasmic sperm injection (ICSI) is used when male factor infertility is present. Research indicates that health outcomes for ICSI‑conceived children are comparable to those from standard IVF after accounting for parental factors.
Bottom line: the science tells us that IVF‑conceived children are, for the most part, just as healthy as their naturally conceived siblings. The small differences that do exist are linked to treatable variables like multiple pregnancies and maternal age, not to the laboratory process itself. Armed with this knowledge, families can make informed choices, clinics can refine protocols, and policymakers can support evidence‑based guidelines.