IVF Success Rate Calculator
Calculate your personalized live-birth rate based on CDC 2023 data and maternal age. Note: This tool uses average national statistics.
Enter your age group and click "Calculate" to see your estimated live-birth rate.
When you hear about couples finally having a baby after IVF, it’s easy to wonder-can this miracle happen every single time? The short answer is no. IVF success rate is a complex metric shaped by many variables, not a blanket 100% guarantee.
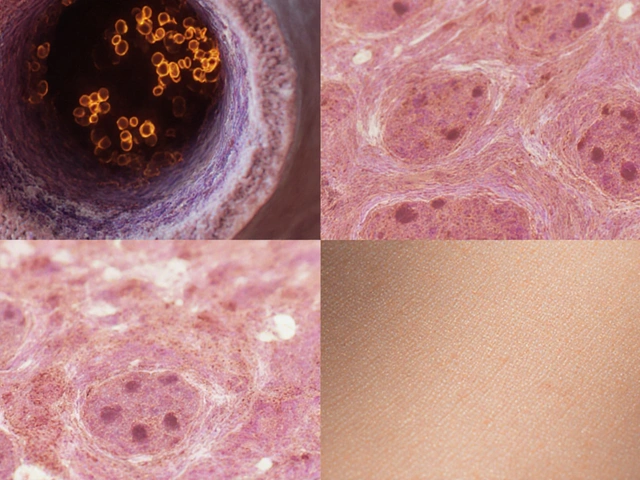
What IVF Actually Is
Invitrofertilization is a medical procedure that combines an egg and sperm outside the body, then transfers the resulting embryo into the uterus. It’s the cornerstone of modern assisted reproductive technology (ART) and has helped millions of families grow, but it’s still a series of carefully timed steps that each carry their own risk of failure.
How Success Is Measured
Clinics report several numbers, and they’re not interchangeable:
- Clinical pregnancy rate: detection of a gestational sac on ultrasound, usually at around six weeks.
- Live‑birth rate: the birth of a living infant, which is the gold‑standard outcome for patients.
- Implantation rate: the proportion of transferred embryos that successfully embed in the uterine lining.
When we talk about “IVF success,” most experts, including the American Society for Reproductive Medicine, refer to the live‑birth rate per cycle started.
Real‑World Statistics
According to the latest CDC ART report (2023 data), the national average live‑birth rate per fresh IVF cycle was about 32% for women under 35, dropping to 11% for women aged 42‑44. Those numbers are averages across thousands of clinics, each with different protocols, experience levels, and patient profiles.
The Society for Assisted Reproductive Technology (SART) tracks similar data and shows a modest upward trend over the past decade, thanks to improvements in embryo culture, better hormonal monitoring, and wider use of preimplantation genetic testing (PGT) to screen for chromosomal abnormalities.
Key Factors That Influence IVF Success
Success isn’t a simple flip‑of‑a‑coin. Here are the biggest drivers:
- Maternal age - Egg quality declines sharply after 35, making age the single most predictive factor.
- Embryo quality - Graded on morphology and, when PGT is used, chromosomal normalcy.
- Clinic expertise - High‑volume fertility clinics tend to have better lab standards and higher cumulative live‑birth rates.
- Number of embryos transferred - Transferring more embryos raises pregnancy odds but also increases the risk of multiples.
- Underlying diagnosis - Conditions like severe male factor infertility, diminished ovarian reserve, or uterine abnormalities can lower success.
- Lifestyle factors - Smoking, excessive alcohol, high BMI, and chronic stress can all reduce implantation chances.

Success Rates by Age - A Quick Comparison
| Age Group | Live‑birth Rate | Typical # of Embryos Transferred |
|---|---|---|
| Under 35 | 32% | 1‑2 |
| 35‑37 | 27% | 1‑2 |
| 38‑40 | 21% | 1‑2 |
| 41‑42 | 15% | 1 |
| 43‑44 | 11% | 1 |
The steep decline after 38 illustrates why many specialists recommend earlier intervention for couples planning to delay parenthood.
Myths About a 100% Success Rate
It’s tempting to think that with today’s tech a single IVF cycle will guarantee a baby, but here’s why that’s unrealistic:
- Even the best labs report a range of outcomes-some embryos never implant.
- Technical steps like egg retrieval and sperm injection (ICSI) can fail to produce viable embryos.
- Uterine receptivity is a moving target; a perfectly formed embryo may still encounter a hostile lining.
- Patient‑specific issues-auto‑immune disorders, endometriosis, or unexplained infertility-can blunt success despite flawless lab work.
Depicting IVF as a “sure‑thing” overlooks the emotional, financial, and physical toll of repeated cycles.
Practical Tips to Maximize Your Odds
- Start early. If you’re over 35, schedule a consultation as soon as possible.
- Choose a reputable clinic. Look for high cumulative live‑birth rates and transparent reporting.
- Consider PGT. Screening embryos for chromosomal health can raise live‑birth chances, especially for older patients.
- Optimize lifestyle. Aim for a BMI of 18‑25, quit smoking, limit caffeine, and manage stress.
- Follow medication protocols precisely. Missing a dose can shift hormone levels enough to affect egg quality.
- Ask about frozen‑embryo transfers. Frozen cycles often yield comparable or better outcomes than fresh transfers.

When IVF May Not Be the Right Choice
Some situations have very low odds even with multiple cycles:
- Severe diminished ovarian reserve (AMH < 0.5ng/mL).
- Uterine factor infertility that cannot be corrected surgically.
- Genetic conditions where all embryos carry a serious disease.
Patients in these scenarios might explore alternatives like donor eggs, gestational surrogacy, or adoption.
Bottom Line
IVF is a powerful tool, but it’s not a guarantee. Real‑world live‑birth rates hover between 30% and 10% depending on age, health, and clinic quality. Understanding the numbers, debunking myths, and actively optimizing every controllable factor give you the best shot at turning a hopeful cycle into a happy delivery.
Frequently Asked Questions
What is the average IVF success rate?
Across the United States, the average live‑birth rate per fresh IVF cycle is about 32% for women under 35 and drops to roughly 11% for women aged 42‑44, according to the 2023 CDC report.
Does using frozen embryos improve success?
Yes. Many studies, including those cited by SART, show that frozen‑embryo transfers have similar or slightly higher live‑birth rates than fresh transfers, partly because the uterine environment is more stable.
How much does age affect IVF outcomes?
Age is the strongest predictor. Women under 35 have roughly a 30‑35% chance per cycle; by age 40 the chance falls to about 20%, and after 42 it can dip below 15%.
Can preimplantation genetic testing boost my odds?
PGT can increase live‑birth rates, especially for older patients or those with recurrent miscarriage, by ensuring only chromosomally normal embryos are transferred.
What are the main reasons a cycle fails?
Common causes include poor egg quality, abnormal sperm, low embryo quality, uterine receptivity issues, and suboptimal hormone levels during stimulation.