IVF Success Rate Estimator
IVF Success Rate Calculator
Estimate your personalized IVF success rate based on your age, egg quality, and treatment options. This calculator uses clinical data from recent studies to provide realistic expectations.
Enter your information to see your estimated success rate.
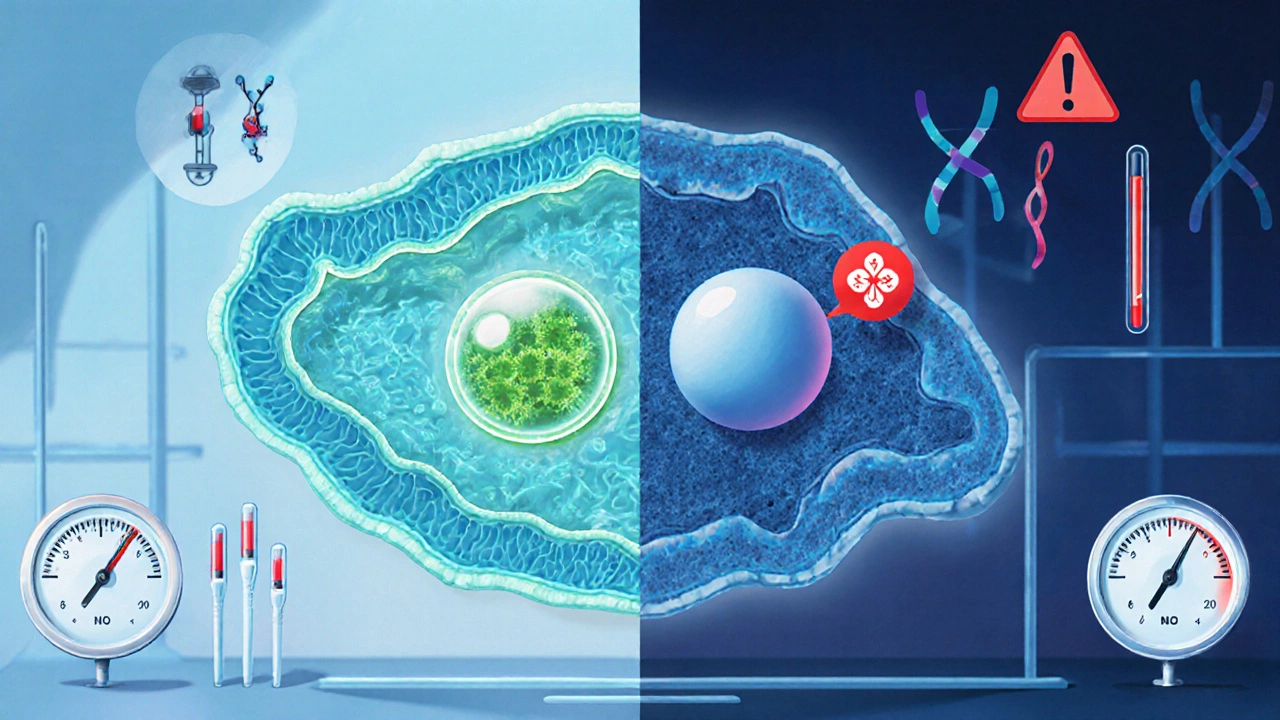
When you hear the term IVF is in‑vitro fertilization, a lab‑based method that joins an egg and sperm outside the body to create an embryo, you probably picture a hopeful couple holding a baby‑carrying passport. The reality, however, is that many couples face a stubborn roadblock: the embryo often never implants. That implantation hurdle is the single biggest problem dragging down overall success rates.
Key Takeaways
- Implantation failure, not egg retrieval, is the primary bottleneck in IVF outcomes.
- Age, egg quality, uterine receptivity, and genetic abnormalities account for >70% of implantation failures.
- Pre‑implantation genetic testing (PGT‑A), personalized ovarian stimulation, and endometrial assessment can boost chances by 10‑15%.
- Choosing a clinic with high lab standards and transparent success metrics matters as much as the medical protocol.
- A simple checklist helps patients spot red flags before signing a treatment contract.
Why IVF Success Rates Stall
Worldwide IVF live‑birth rates hover around 30% per cycle for women under 35, dropping to under 10% after 42. Those numbers look good at first glance, but they hide a crucial detail: nearly half of all retrieved eggs turn into embryos, yet only a fraction of those embryos ever reach the uterus, and an even smaller slice actually implant.
In plain language, the process works well until the embryo meets the lining of the uterus. If the lining isn’t receptive or the embryo carries hidden genetic errors, the body simply rejects it. That rejection is what most patients label as “the biggest problem with IVF.”
Major Factors Behind Implantation Failure
Understanding the why helps you target the how. Below are the five biggest contributors, each backed by recent clinical data (2023‑2025).
- Maternal Age & Egg Quality - Egg mitochondria deteriorate after 35, raising aneuploidy rates to 60% in women over 40. Aneuploid embryos often fail to implant.
- Uterine Receptivity - The window of implantation (WOI) is a 48‑hour period when the endometrium expresses specific proteins (integrins, LIF). Misaligned WOI leads to a 25% drop in live births.
- Genetic Abnormalities - Even morphologically good embryos can harbor chromosomal issues. PGT‑A catches these, improving implantation by ~12%.
- Ovarian Stimulation Protocols - Aggressive gonadotropin doses raise estrogen levels, which may alter endometrial gene expression and shrink the WOI.
- Lab & Embryology Practices - Temperature swings, culture media variations, and suboptimal embryo grading can reduce blastocyst viability.
How a fertility clinic a medical center that offers assisted reproductive technologies Tackles the Problem
Top clinics adopt a three‑pronged approach: (1) personalize ovarian stimulation, (2) assess endometrial receptivity, and (3) apply genetic screening when appropriate.
- Personalized Stimulation: Using AMH and AFC scores, doctors select low‑dose protocols for older patients to keep estrogen in a “friendly” range (250‑400pg/mL).
- Endometrial Receptivity Analysis (ERA): A tiny biopsy taken a week before transfer reveals the exact WOI. Timing the embryo transfer to that window lifts live‑birth odds by 8‑10%.
- Pre‑implantation Genetic Testing for Aneuploidies (PGT‑A): Biopsying 5‑10 cells from the trophectoderm of a blastocyst identifies chromosomal errors. Transferring only euploid embryos halves miscarriage risk.
When these steps are combined, clinics report cumulative live‑birth rates of 45-55% after three cycles - a stark improvement over the raw average.
Comparison of IVF Success‑Boosting Strategies
| Strategy | Average Live‑Birth Increase | Cost Increment (USD) | Typical Patient Profile |
|---|---|---|---|
| Low‑dose Stimulation | +5‑7% | +$1,200 | Women >38, low AMH |
| Endometrial Receptivity Analysis | +8‑10% | +$2,500 | Repeated implantation failure (≥2 cycles) |
| PGT‑A (aneuploidy screening) | +12‑15% | +$3,800 | Maternal age >35 or recurrent miscarriage |
| Time‑Lapse Embryo Imaging | +3‑4% | +$1,600 | Clinics with high embryo volume |
| Adjunctive Immunotherapy | +2‑5% | +$900 | Elevated NK cell activity (rare) |

Patient Checklist: Spotting Red Flags Before Starting IVF
- Ask for the clinic’s cumulative live‑birth rate per age group, not just per‑cycle numbers.
- Verify that the embryology lab follows ISO15189 standards and records temperature logs.
- Confirm whether they offer personalized stimulation plans based on AMH and AFC.
- Check if they perform ERA or other receptivity testing when you have ≥2 failed transfers.
- Make sure costs for PGT‑A, ERA, and any adjunct treatments are disclosed up front.
Cross‑checking these items can save you months of frustration and thousands of dollars.
Beyond IVF: When to Consider Alternative Paths
If implantation remains a stubborn hurdle after three cycles, looking at alternatives isn’t a defeat; it’s a strategic pivot.
- IUI (Intrauterine Insemination): Works well for mild male factor or unexplained infertility, with lower cost and no lab‑stage embryos.
- Donor Egg Programs: Bypass egg quality issues entirely; live‑birth rates climb to 60%+ for women over 45.
- Adoption or Surrogacy: For couples facing uterine-factor infertility, these routes bypass the implantation step.
Choosing any of these paths should be a discussed decision with a qualified reproductive endocrinologist.
Frequently Asked Questions
Why do embryos fail to implant even when they look perfect?
Morphology only tells part of the story. Hidden chromosomal errors, an out‑of‑phase endometrial window, or subtle hormonal imbalances can cause a seemingly healthy blastocyst to be rejected by the uterus.
Is PGT‑A worth the extra cost for women under 35?
For most women under 35 with normal ovarian reserve, the baseline aneuploidy rate is under 30%, so the cost‑benefit ratio is modest. However, if you have a history of miscarriage or a partner with known genetic issues, PGT‑A can meaningfully raise success odds.
How does an ERA test work, and is it painful?
A tiny pipette collects a few dozen cells from the uterine lining about a week before a planned transfer. The procedure is similar to a Pap smear - brief, mild discomfort, and no anesthesia required.
Can lifestyle changes improve implantation rates?
Yes. Maintaining a BMI between 18‑25, quitting smoking, limiting caffeine to <10mg/day, and reducing stress (e.g., yoga, mindfulness) are linked to a 5‑8% bump in live‑birth odds.
What should I look for in a clinic’s lab to avoid embryo loss?
Ask for ISO15189 accreditation, continuous temperature and gas monitoring logs, and whether they use time‑lapse imaging or sequential media. Transparent labs usually publish their embryo grading criteria.



